
I found the following information on the web and found it quite interesting. I've asked the doctor if there was anything I could have done to prevent the access from clotting. They said 'no'. I hope to talk to the new vascular surgeon about this and hopefully get some answers. Also, I have this nagging dissatisfaction with the information I've been given about the old access. They do nothing about the clots that have caused this blockage. They say they can't go anywhere or be a problem. That doesn't make sense to me. I will keep searching for answers.
What is access clotting?
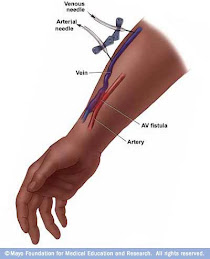
Answer: “Clotting” of the dialysis access is a common problem for the hemodialysis patient. Also known as thrombosis, clotting is actually the conversion of the liquid blood into a solid plug in the dialysis access. This plug stops the blood from moving freely through the access. Although clotting of blood when it is outside the body is normal and protects us from excessive bleeding when we are injured, clotting of blood inside a blood vessel is abnormal and is usually the result of sluggish blood flow through the vessel. There are a number of things that can cause sluggish access blood flow including poor blood flow into the access, narrowing in the outflow of the access, compression of the access and blood pressure drops.
Poor flow into the access is sometimes a technical problem with the original connection of the artery to the vein (on a fistula) or of the artery to the graft material (on an AV graft) at the time of surgery. Sometimes the blood flow into the access is poor because of diseased arteries due to diabetes, high blood pressure, older age or history of smoking. Narrowing of the outflow of the access occurs when scar tissue forms at the connection of the graft material and the vein. Sometimes the narrowing may already be present in the deeper veins at the time of the surgical placement of the dialysis access, especially if a patient previously had a dialysis catheter in the deeper vein, such as a subclavian vein.
Compression of the access may be accidental if, for example, a patient sleeps on the arm with the access or the patient is under anesthesia for a surgical procedure and the arm with the access is not positioned properly or if a blood pressure is taken in the dialysis access arm. Compression of the access may be intentional in an effort to stop prolonged bleeding from the access site after the needles are withdrawn following a dialysis procedure. In that setting, care must be taken to avoid excessive or prolonged pressure, especially if a mechanical compression device is used. Blood pressure drops occur when too much fluid is removed during dialysis. This may happen if a person gains muscle or fat weight and needs a dry weight increase. These blood pressure drops may also occur when a large volume of fluid is removed at a single dialysis treatment. If the blood pressure falls while the patient is still on dialysis, lying back helps to preserve flow through the access and administration of fluid will help raise blood pressure back to normal. Sometimes, patients experience blood pressure drops after the dialysis treatment is finished and they have already gone home. If this occurs, the patient should also lie back to help preserve flow through the access and take fluids by mouth to help raise the blood pressure to normal.
There are several things that a patient can do to help prevent clotting of the dialysis access. First, patients should attend all dialysis treatments and undergo routine monitoring of the blood flow through the dialysis access. If the flow decreases, a test should be performed to determine the cause of the problem. Problems with the inflow to the fistula or graft can be referred to the surgeon for surgical repair. Problems with the outflow of the access may be able to be corrected in the radiology department with “ballooning” or angioplasty of the narrowed section of the vein.
In addition, patients should be careful of the amount of fluid consumed and weight gained between dialysis treatments. Controlling the dietary salt intake can help to decrease thirst and prevent large fluid gains. Patients should also be aware of blood pressure decreases on dialysis and report them to their nephrologist. The nephrologist may increase the dry weight or re-adjust blood pressure medications to help to prevent future blood pressure drops.
As every hemodialysis patient knows, their vascular access it literally their “lifeline” which must be treated with the utmost care to keep it functioning properly. Clotting of a fistula or graft is usually due to an identifiable reason, and treatment of a clotted access should include, in addition to removing the clot, an investigation and correction of that reason, if possible, so that the access does not soon clot again. Unfortunately, some clotted accesses cannot be fixed, but in such cases the nephrology practitioner, surgeon and patient should try to learn the causes of the clotted access before planning any new access.






No comments:
Post a Comment